Foot pain affects nearly all people at one time or another. It can also lead to other musculoskeletal problems such as ankle, knee and back pain (Hill et al., 2008). This pain negatively affects one’s quality of life and ability to enjoy workouts and/or maintain a regular program of exercise. One of the most common sources of foot pain is plantar fasciitis, a condition where the connective tissue on the underside of the foot becomes irritated and painful as a result of an injury, overuse or misuse.
Staying Within Your Scope of Practice
It is not appropriate, or your job, as a fitness professional to diagnose plantar fasciitis. That is the responsibility of licensed medical professionals who are trained in the assessment and diagnosis of such conditions. However, because many of your clients will come to you with a diagnosis of plantar fasciitis, it is your responsibility (and well within your scope of practice) to understand what plantar fasciitis is, how it is caused, and what you can do to address underlying musculoskeletal problems to help clients alleviate their painful symptoms (American Council on Exercise, 2010).
What Is Plantar Fasciitis?
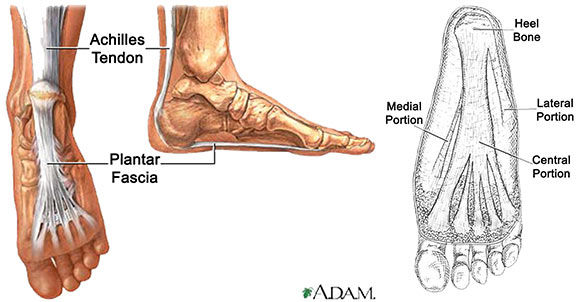
The plantar fascia is a system of connective tissue that runs from your heel to just behind your toes (Figure 1). During weightbearing activities, such as walking or running, your body weight is transferred onto your foot from your heel to your toes (which results in your toes moving away from your heel). This spreading out of the foot places tension on the plantar fascia because it connects those two parts. If the tension on this structure is too great or is not dispersed evenly, the plantar fascia can develop microtears and become irritated and painful, resulting in a condition called plantar fasciitis (Schamberger, 2002).
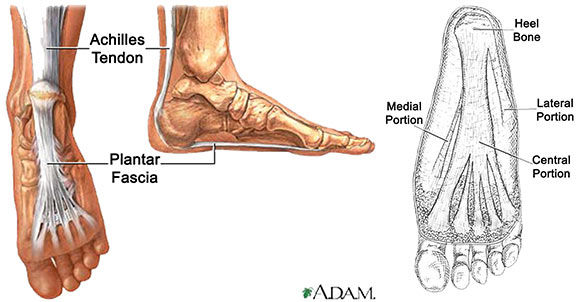
Figure 1: Plantar Fascia
How Do People Get It?
When a person is walking or running, the body travels forward over the foot of the weightbearing leg. The body also moves across the foot from side to side so that its weight can be transferred left to right (and vice versa) as the person takes alternating steps. The plantar fascia is ideally designed to help the foot accept the body’s weight as a person makes these two movements (Price and Bratcher, 2010). As you can see in Figure 1, the plantar fascia fans out and widens as it extends forward from the heel to the toes. This brilliant design enables the plantar fascia to help the feet accept a person’s body weight from above and transfer it forward and from side to side. As long as your body is making these forward and side-to-side movements correctly, the plantar fascia can function well and the tissue remains healthy.
However, if a person has musculoskeletal issues that prevent the proper transfer of body weight forward and from side to side, certain areas of the plantar fascia can get overworked and injured. Two of the most common musculoskeletal imbalances that can affect the correct functioning of the foot and ankle are overpronation and lack of dorsiflexion (American Council on Exercise, 2010). Overpronation is characterized by the foot and ankle collapsing inward toward the midline of the body. A lack of dorsiflexion is characterized by the inability of the ankle to bend forward in order for the lower leg to come forward over the foot. These two imbalances are inherently linked and can cause a lot of damage to the plantar fascia. When a person’s body weight shifts across the foot too much toward the midline of the body (as what happens as a result of overpronation), it prevents the foot and ankle from effectively transferring the body weight forward over the foot (the ability to dorsiflex). This means that the plantar fascia, which is designed to evenly accept weight forward and from side to side, is overstressed with side-to-side motion and becomes susceptible to injury. When a person with the imbalances described above engages in activities that repeatedly stress the plantar fascia in this manner, the damage caused to this tissue can become severe and chronic.
Can Orthotics or Arch Supports Help?
The temporary use of orthotics or arch supports can often be helpful in alleviating the painful symptoms of plantar fasciitis. These types of shoe inserts provide a “crutch” to the foot in the form of artificial support designed to reduce overpronation, which in turn can increase dorsiflexion. Clients may want to consider using arch supports to minimize their pain while you work together to address their underlying musculoskeletal imbalances. However, unless they have been otherwise directed by a licensed health professional, it is not advisable for clients to utilize orthotics or arch supports as a long-term solution to plantar fasciitis, as this will only serve to weaken the underlying structures of their feet.
What Can Be Done To Help Alleviate It?
The key to alleviating plantar fasciitis is to address dysfunctional soft tissue structures that may be having an impact on the ability of the foot and ankle to dorsiflex. To enable this to happen the feet, calves, and hip flexors must all be working correctly to ensure that weight can be displaced forward over the plantar fascia and not just from side to side. Retraining these areas can help prevent or alleviate plantar fasciitis.
Feet
The plantar fascia must be able to accept weight from the heel forward to the toes in order for the lower leg to come over the foot (i.e., dorsiflex). When a person overpronates, the plantar fascia does not get the opportunity to accept tension forward, but rather “twists” from side to side. Retraining the plantar fascia to accept body weight as it transfers in a forward direction will help alleviate the effects of plantar fasciitis.
Calves
To dorsiflex, the lower leg must travel forward over the foot as the ankle bends. As this happens, the calf muscles (i.e., soleus and gastrocnemius), which attach to the Achilles tendon (and share an attachment on the heel bone with the plantar fascia), lengthen under the weight of the body to control forward movement (Gray, 1995). The tension created on the calf muscles and Achilles tendon also creates tension on the plantar fascia. Hence, retraining the calves to lengthen effectively to accept body weight as it travels forward will not only help increase dorsiflexion, but also help control the body as it travels forward over the foot and plantar fascia.
Hip Flexors
The hip flexors work in conjunction with the calf muscles and structures of the foot to allow dorsiflexion. When a person is walking, the hip flexors of the weightbearing leg lengthen under the load of the person’s weight as the body travels forward over the foot. As such, correct function of the hip flexors is inherently linked to the correct function of the calves and feet (Myers, 2001). Retraining the hip flexors to be able to lengthen effectively (along with the calf muscles) as the hip/leg travels into extension will help promote dorsiflexion and alleviate the effects of plantar fasciitis.
What Corrective Exercise Strategies Should Clients Use?
Any successful corrective exercise program should begin with a series of self-myofascial release (SMR) techniques to help rejuvenate and regenerate the tissues that have been damaged by an injury or underlying musculoskeletal imbalance (Rolf, 1989). Therefore, before attempting any stretching exercises for the feet, calves and/or hip flexors, have your client perform the following SMR exercises.

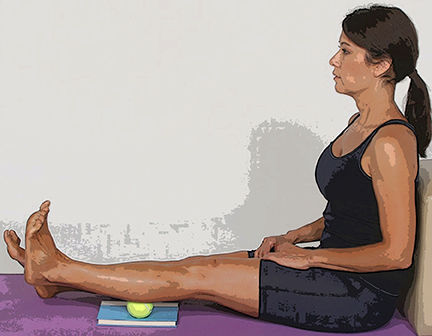
SMR #1 - Golf Ball Roll
Roll the underside of each foot for 30 to 60 seconds at least once a day.
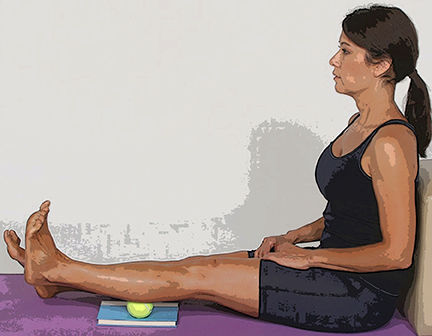
SMR #2 - Calf Massage
Use a tennis ball or baseball to massage any sore spots on the backs of each lower leg for one to two minutes at least once a day.

SMR #3 - Foam Roller on Hip Flexors
Roll the front of each hip and top of each leg for one to two minutes at least once a day.
Once the tissues in these areas have been warmed up, you can progress your client to stretching exercises. All of the following stretching exercises are performed when the client is standing, which ensures that the target muscle(s) and structures learn to lengthen while under the load of gravity. This is very important because each of these structures must be able to lengthen as they would in real-life circumstances, when the plantar fascia is most likely to be placed under stress or injured (e.g., when standing, walking or running) (Price and Bratcher, 2010).
Stretch #1 - Foot and Toe Stretch
Most of the soft-tissue structures on the underside of the foot, including the plantar fascia, travel from the heel all the way to the toes. As such, it is important to involve the toes when stretching the feet.
Place one foot forward with the toes up against the base of a wall or half foam roller. Gently bend the knee forward or toward the wall to increase the stretch felt under the foot. Make sure the foot and ankle do not collapse inward (i.e., overpronate) while performing this exercise. Stretch each foot for 20 to 30 seconds at least once a day.
Stretch #2 - Calf Stretch on BOSU
Performing a standing calf stretch helps promote better dorsiflexion. However, stretching the calf muscles on a BOSU Balance Trainer enables the heel to drop lower than the toes and increases the effectiveness of this exercise.
Stand in a split stance on a BOSU Balance Trainer with the hands on a wall or desk to assist with balance. Push the heel of the back foot down to feel the stretch in the calf muscles. Perform this stretch twice, once with a bent knee and once with a straight knee, to address both the soleus and gastrocnemius muscles of the calf. Be sure your client does not overpronate as he or she performs this exercise. If tension is felt in the front of the ankle, regress to the SMR technique for the calf described above. Perform this stretch on each leg for 30 to 60 seconds once a day.
Stretch #3 - Step Back With Arm Raise
Once the foot and calf muscles have been retrained to help create better dorsiflexion, the client can add the hip flexor muscles to create an integrated movement that addresses all three muscles at once. This exercise helps clients learn to transfer body weight over the hips and foot and ankle during all weightbearing activities.
Take a step back with the right foot and raise the right arm overhead. Keep the feet straight and hips pointed forward. Step back and squeeze the right buttocks to help increase the stretch felt in the right hip flexors and right calf. If your client feels this stretch in the lower back instead of the intended areas, regress to the Foam Roller on Hip Flexors exercise (shown above). Perform this stretch on both sides, three to five times on each side, at least once a day.
Conclusion
Understanding what a diagnosis of plantar fasciitis means is essential to helping clients overcome the problem. While it is not within your scope of practice to determine if a client has plantar fasciitis, you can use your knowledge of what causes it to address problematic muscle and soft tissue imbalances. The whole body works as an integrated system of parts and the application of effective corrective exercises will enable you to address the underlying causes of this condition and alleviate your client’s pain.
Become a BioMechanics Method® Corrective Exercise Specialist

Want to learn more about how you can help your clients who have low-back pain? The BioMechanics Method® Corrective Exercise Specialist online course (TBMM-CES) is specifically designed to give fitness professionals a step-by-step process for working with clients who experience muscle and joint pain. Created by Justin Price, one of the top musculoskeletal assessment and corrective exercise experts in the world, this course will give you the postural assessment, anatomy, corrective exercise and program design skills necessary to help clients become pain free. This self-paced study course is valued at 8.0 ACE CECs and includes digital textbooks, videos and online quizzes.
References
American Council on Exercise (2010). ACE Personal Trainer Manual, 4th edition. San Diego, Calif.: American Council on Exercise.
Gray, H. (1995). Gray’s Anatomy. New York: Barnes & Noble Books.
Hill, C. et al. (2008). Prevalence and correlates of foot pain in a population-based study. Journal of Foot and Ankle Research, July, 1, 2.
Myers, T. (2001). Anatomy Trains: Myofascial Meridians for Manual and Movement Therapists. Edinburgh: Churchill Livingstone.
Price, J. and Bratcher, M. (2010). The BioMechanics Method Corrective Exercise Educational Program. San Diego, Calif.: The BioMechanics Press.
Rolf, I.P. (1989). Rolfing: Reestablishing the Natural Alignment and Structural Integration of the Human Body for Vitality and Well-Being (revised edition). Rochester, Vt.: Healing Arts Press.
Schamberger, W. (2002). The Malalignment Syndrome: Implications for Medicine and Sport. London: Churchill Livingstone.

 by
by